A young man with malaise and dyspnea
Jennifer Keen MD, Internal Medicine Resident
Laura Hinkle MD, Assistant Professor of Clinical Medicine
Indiana University School of Medicine
Case:
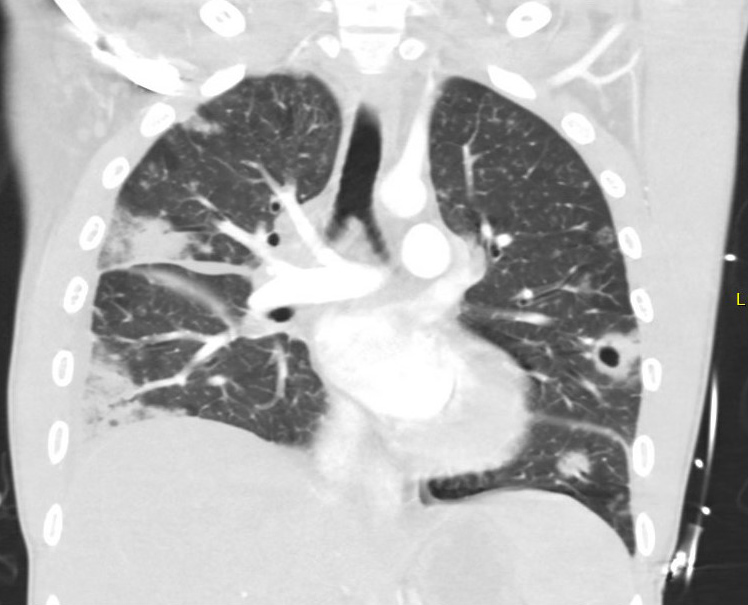
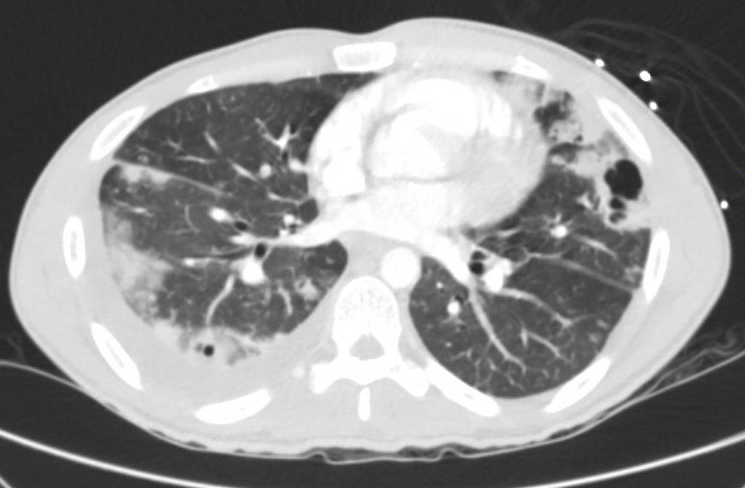
A 26-year-old male IV drug user presented to the hospital with dyspnea and abdominal pain. He was emergently intubated on arrival due to respiratory distress. His family provided additional history that he had exhibited progressive weight loss and fatigue over the past several weeks. Chest CT images are shown below.
What is the most likely diagnosis based on the image?
- Tuberculosis
- Pulmonary embolism with infarction
- Rheumatoid nodules
- Septic emboli
Answer 4 Septic emboli
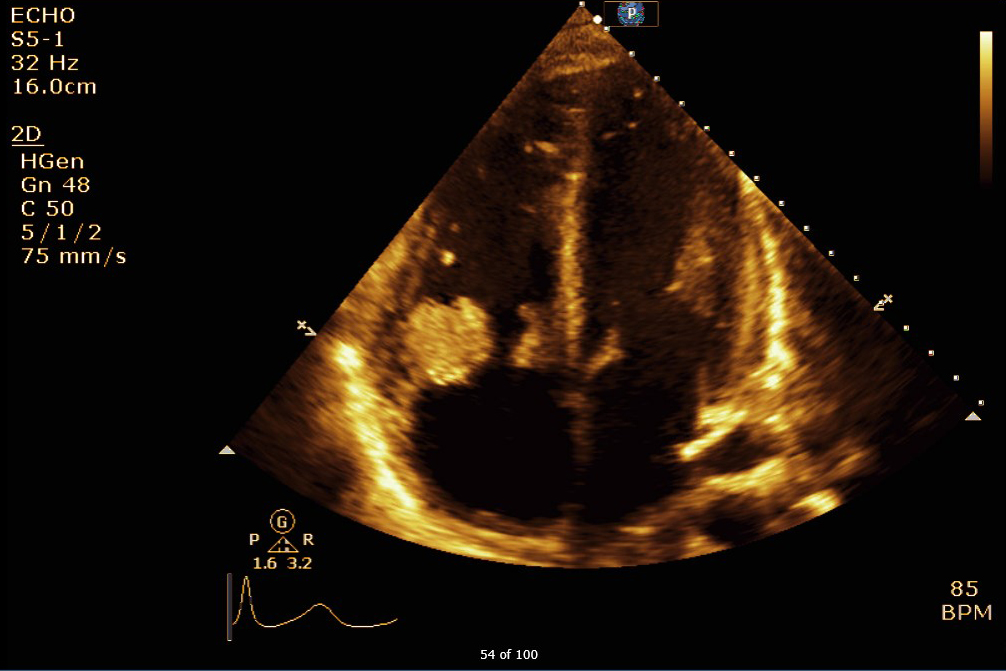
Chest CT imaging revealed bilateral peripheral pulmonary nodules, many of which were cavitary, as well as mediastinal lymphadenopathy. The patient was found to have Methicillin sensitive Staphylococcus aureus (MSSA) bacteremia. An transthoracic echocardiogram (TTE) revealed large mobile masses attached to the tricuspid valve (the largest measuring up to 2.8 cm by 2.1 cm) with associated moderate to severe tricuspid regurgitation.
Peripheral cavitary nodules in the setting of IV drug use is suspicious for septic emboili, and given this patient's blood cultures and TTE findings, a diagnosis of bacterial endocarditis was made. Tuberculosis would exhibit upper lobar preference, which was not seen in this patient's imaging. Rheumatologic nodules would be associated with additional findings such as skin nodules. Pulmonary embolism can result in infarction and necrosis with subsequent cavitary formation, often in the periphery and without lobar preference. Although pulmonary embolism with infarction is possible, the patient's presentation (including IVDU history, blood cultures, and TTE findings) was more consistent with septic emboli due to endocarditis.
Pulmonary septic emboli are common in right-sided endocarditis and occur in up to 75% of patients with tricuspid valve involvement. They may also arise from sites of thrombophlebitis in peripheral veins or in Lemierre's syndrome. Radiographic findings of septic emboli can include not only cavitary lesions as seen in our patient, but also abscesses or infarction. Suspicion for septic emboli as the etiology of these radiographic findings should increase in the setting of IVDU, positive blood cultures, or new cardiac murmurs.
Cavitary nodules can be present in many diseases, with clinical history and exam often providing guidance to the correct diagnosis. These diseases can broadly be categorized as infectious and non-infectious. Infectious etiologies include pulmonary abscesses or necrotizing lobar pneumonia involving anaerobic bacteria, mycobacterium, fungi, parasites, or septic emboli. Non-infectious processes include pulmonary embolism with infarction, vasculitis, malignancies, cysts with air-fluid levels, bronchiectasis, cryptogenic organizing pneumonia, sarcoidosis, rheumatoid nodules, or foreign body aspiration. A helpful mnemonic for cavitary nodular lesions is CAVITY – Cancer, Autoimmune, Vascular, Infection, Trauma, Youth (e.g. congenital pulmonary airway malformation).
Gadkowski LB, Stout JE. Cavitary Pulmonary Disease. Clinical Microbiology Reviews. 2008;21(2):305–333
Muller KA, Zurn CS, Patrik H, et al. Massive haemoptysis in an intravenous drug user with infective tricuspid valve endocarditis. BMJ Case Rep 2010; 2010.