Chronic Cough and Dyspnea
Mandeep Singh, MD1; Evgeniya Angelova, MD2, PhD; Shawn Nishi, MD1
1Department of Internal Medicine, Division of Pulmonary Critical Care and Sleep Medicine
2Department of Pathology
University of Texas Medical Branch
301 University Boulevard
Galveston, TX 77555-0561
Case
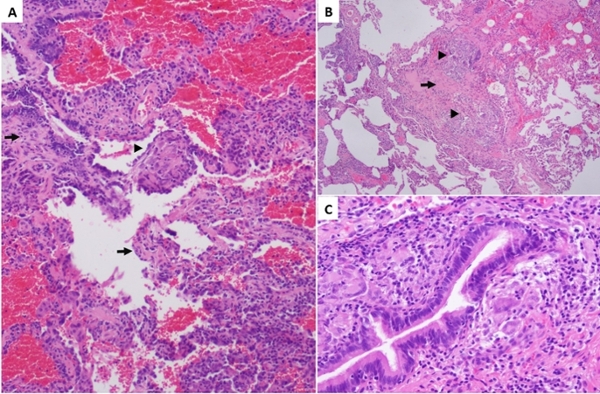
A 65-year-old Caucasian female is referred to the pulmonary clinic with progressively worsening of productive cough and shortness of breath for 3 months. She had failed trials of antibiotics, nasal steroids and antihistamines. She denies GERD, history of asthma or recent illness or travel. She is a lifelong non-smoker and has a desk job. Initial spirometry revealed FEV1 2.03 L (84% predicted), FVC 2.51 L (80% predicted), FEV1/FCV 0.81 and exertional desaturation requiring 4L nasal cannula to maintain SpO2 greater than 90%. Initial (Figure 1) and repeat (Figure 2 and 3) CT thorax images are shown. Our patient was referred for VATS lung biopsy (Figure 4).
Figure 1
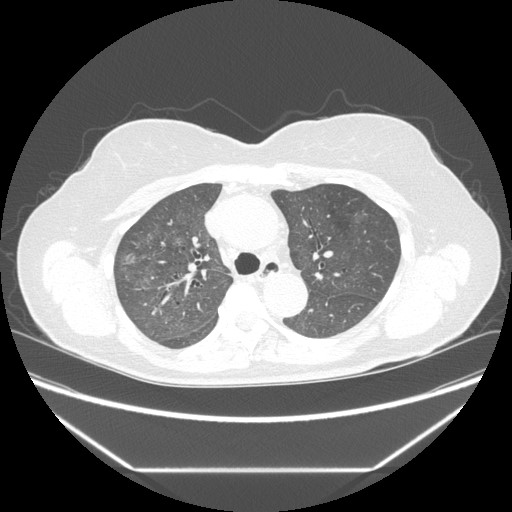
Figure 2
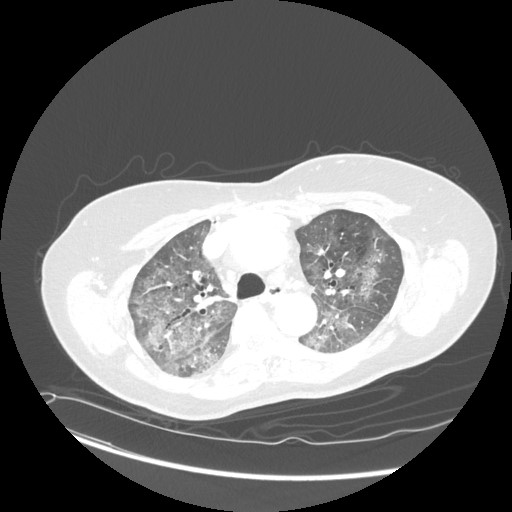
Figure3
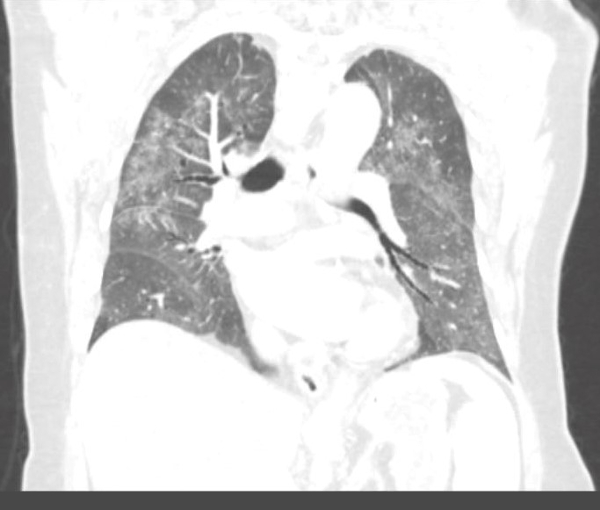
Figure 4
Question
What is the most likely diagnosis?
- Non-specific interstitial pneumonia
- Cryptogenic organizing pneumonia
- Hypersensitivity pneumonitis
- Desquamative interstitial pneumonia
Answer: C. Hypersensitivity Pneumonitis
Figure 1. Subtle scattered nodules and ground glass opacities mainly in the upper lobes.
Figure 2. Ground glass opacities involving the upper lobes and lower (not pictured), with subpleural sparing and mosaic attenuation.
Figure 3. More consolidation with sub-pleural sparing in the upper lobes and mosaic attenuation in the lower lobes.
Figure 4. Pathologic findings: A. Airway centered lymphocytic infiltration with thickening of the alveolar septa (arrows) and loose granuloma (arrowhead) (hematoxylin-eosin, 100x); B. Vaguely formed nonnecrotizing granulomata in the interstitium (arrowheads) with fibrosis (arrows) (hematoxylin-eosin, 40x); C. Peribronchiolar giant cells with poorly formed granulomas and mononuclear infiltration (hematoxylin-eosin, 200x).
Discussion
Upon further interview, our patient admitted to having a pet-bird for years. These radiologic and histopathologic findings along with a history of exposure to organic antigens in a symptomatic patient are consistent with the diagnosis of subacute hypersensitivity pneumonitis (HP). The patient was started on steroids and relocated her pet bird. Four months later, her symptoms of cough and dyspnea were significantly improved.
Subacute HP is a diffuse granulomatous interstitial lung disease caused by inhalation of various antigenic organic particles. Repeated antigen exposure causes immunologic sensitization of the host to the antigen and immune-mediated damage to the lung. These antigens are presented by macrophages and dendritic cells, resulting in the differentiation of CD4 lymphocytes towards Th1 cells. Cytokines are secreted by Th1 lymphocytes and macrophages which promote granuloma formation. There is interstitial and peribronchiolar lymphocyte accumulation.
Patients usually present with insidious onset of dyspnea, fatigue and cough over weeks to months. Pulmonary function tests reveal restrictive pattern and reduction of the carbon monoxide diffusion capacity (DLCO). Bronchoalveolar lavage findings include an increase in the total cell count with a marked lymphocytosis. The CD4+/CD8+ ratio is classically less than 1. Options for tissue sampling include transbronchial lung biopsy, transbronchial cryobiopsy and surgical lung biopsy with a diagnostic yield of 64, 84 and 91% respectively. Histopathologic findings usually consist of bronchiolocentric lymphohistiocytic interstitial pneumonia, chronic bronchiolitis and small, poorly formed, nonnecrotizing granulomas.
Differential diagnosis of CT findings of ground glass opacities includes: 1) Non-specific interstitial pneumonia: in this case presence of centrilobular nodules make it less likely; 2) Cryptogenic organizing pneumonia: although ground glass opacities may be present, patchy consolidation especially in subpleural areas is a dominant feature; 3) Desquamative interstitial pneumonia: ground glass opacities are usually basilar or subpleural and more than 90% patients are smokers which is not consistent with this case.
Diagnosing ILD requires a high index of clinical suspicion, particularly for HP. A thorough history of exposure to antigens at home, work, or related to hobbies must be obtained. Removal of the causative agent, if possible, remains the cornerstone of management. Randomized controlled trials are lacking for all the pharmacotherapeutic agents used for treatment of HP. Systemic corticosteroids are used most often with the aim for lowest-possible dose and shortest duration. Immuno-modulating agents (e.g. azathioprine, mycophenolate) and lung transplantation may be considered in patients with progressive disease. The presence of fibrosis at lung biopsy or HRCT scan is a poor prognostic sign.
References:
- Selman M. Hypersensitivity pneumonitis: insights in diagnosis and pathobiology. Am J Respir Crit Care Med. 2012; 186: 314–324.
- Prince JE, Kheradmand F, Corry DB. 16. Immunologic lung disease. J Allergy Clin Immunol. 2003; 111(2 Suppl): S613–S623.
- Silva C.I., Churg A., Muller N.L. Hypersensitivity pneumonitis: spectrum of high-resolution CT and pathologic findings. Am J Roentgenol. 2007; 188(2): 334–344.
- Cormier Y, Belanger J, Laviolette M. Prognostic significance of bronchoalveolar lymphocytosis in farmer’s lung. Am Rev Respir Dis. 1987; 135(3): 692–695.
- Vasakova M, Morell F, Walsh S, et al. Hypersensitivity pneumonitis: perspectives in diagnosis and management. Am J Respir Crit Care Med. 2017; 196(6): 680–689.



