Colours Don't Lie
Dr Anshul Jain
Assistant Professor, department of pulmonary medicine, ESI PGIMSR,
Basaidarapur, New Delhi, India
Dr Sanket Joshi
DM fellow, department of pulmonary medicine, ESI PGIMSR,
Basaidarapur, New Delhi, India
Dr Mahismita Patro,
Assistant Professor, department of pulmonary medicine, ESI PGIMSR,
Basaidarapur, New Delhi, India
Dr Dipti Gothi (corresponding author),
Professor, department of pulmonary medicine, ESI PGIMSR,
Basaidarapur, New Delhi, India
Case
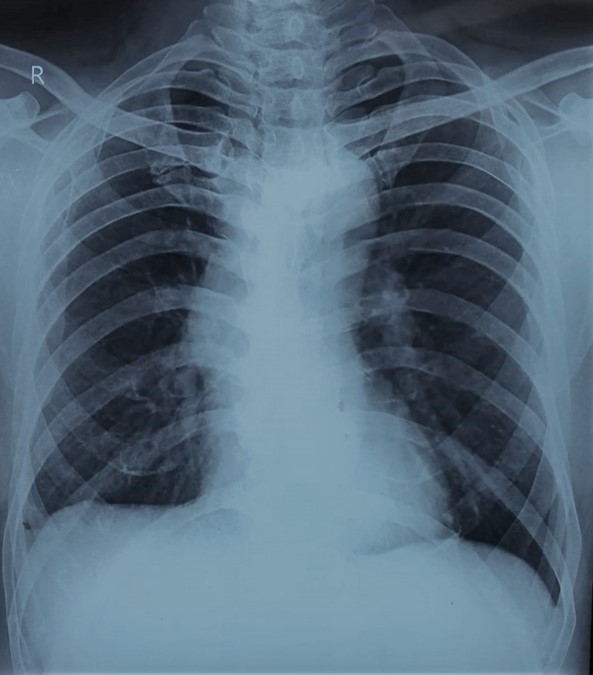
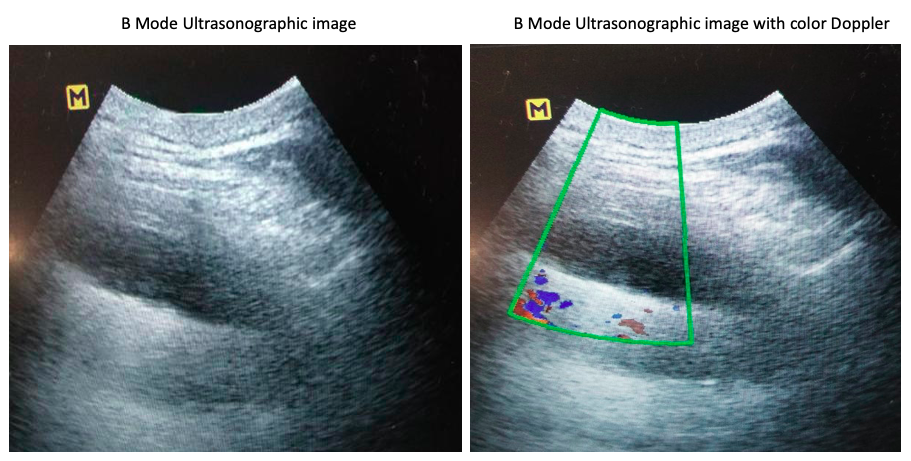
A 39-year-old, man presented to the chest clinic with complaints of right-sided chest pain and mild exertional dyspnea for the last six months. The pain was dull aching in nature and localized to the right lower axillary area and back. There was no history of fever, weight loss or loss of appetite. He had completed six months of anti-tubercular therapy (Rifampicin, isoniazid, ethambutol and pyrazinamide) on a clinical-radiological basis for right-sided pleural effusion one year back. On physical examination his heart rate was 84/min, respiratory rate was 16/min, saturation was 98% at room air by pulse oximetry and blood pressure 134/80 mm of Hg. The respiratory system examination revealed decreased vesicular breath sounds in the right infra-axillary and infra-scapular areas. All the routine blood investigations including haemogram, liver profile and renal profile were within normal limits. His chest radiograph showed blunting of the right costophrenic angle (figure 1). The B mode ultrasonographic image of the right lower chest wall alone and with the colour Doppler is shown in figure 2.
Question
Name the ultrasonographic sign shown in figure 2. What is the diagnosis?
- Presence of fluid colour sign, pleural effusion.
- Absent fluid colour sign, pleural thickening.
- Absent fluid colour sign, pleural effusion.
- Presence of fluid colour sign, pleural thickening.
Answer B. Absent fluid colour sign, pleural thickening
Discussion
The pleural diseases are common clinical conditions and imaging studies are the cornerstone in their management. The chest radiograph is usually the initial diagnostic tool. However, it is less sensitive for the detection of pleural effusion as at least 150 ml of fluid is required in the posterior-anterior view in the erect position[1]. Ultrasound can detect pleural effusion as little as 5 ml with 100% sensitivity[2]. Pleural effusion is seen as an anechoic space between the parietal and visceral pleura during ultrasound.
An important differential of mild pleural effusion (opacity doesn’t exceed the 4th rib on chest radiograph in the erect position) is pleural thickening [3]. But it is difficult to differentiate between the two on chest radiographs alone. The parietal pleural thickness of greater than 3 mm on the chest radiograph indicates pleural thickening, even pleural effusion may have a similar appearance on the chest radiograph [4]. On grey-scale ultrasound, thickening appears as a widened echogenic area of the pleural line with poorly defined margins[5]. However, echogenicity is also seen in the presence of thick fluid, blood or pus. This makes distinguishing pleural thickening difficult even on grey-scale ultrasound. Colour Doppler ultrasound is a useful diagnostic aid in this context.
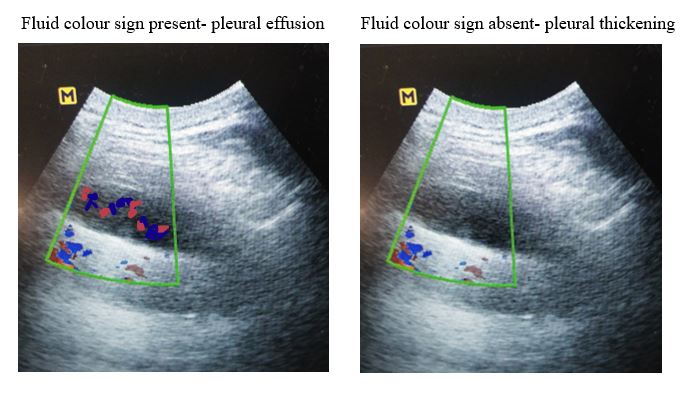
The use of colour Doppler ultrasound is common in cardiovascular imaging studies. It is also utilised in the evaluation of lesions of the peripheral lung, chest wall & mediastinum. But it is underutilized in differentiating pleural effusion from thickening. Pleural fluid produces a colour signal on the colour Doppler ultrasound, known as the ‘fluid colour sign’. Multiple studies have confirmed that if a suspected minimal pleural effusion displays a colour signal on doppler ultrasound, it indicates the presence of fluid. Whereas the absence of colour signal suggests pleural thickening.[6,7] Figure 3 shows the illustrative image of colour Doppler ultrasound differentiating pleural effusion from pleural thickening.
The colour signal in colour Doppler ultrasound is usually due to the presence of vascularity in an organ. But why does pleural fluid produce a colour signal? It is hypothesised that a colour signal may appear artifactually in anechoic regions without blood flow because of the transmission from adjacent tissue motion. The motion signal is likely to be transmitted from the liver, diaphragm, and lung with respiration and heart contraction. It is also possible that the colour signal arises from the relative motion of the components within the pleural effusion.[8] In their study, Hasan and colleagues evaluated the performance of the colour doppler sign in diagnosing pleural thickening using thoracocentesis as the Gold standard in forty patients[6]. They found fluid colour sign had a specificity of 100%, a sensitivity of 91% and an accuracy is 95% for the diagnosis of pleural thickening [7].
In our case, the patient was diagnosed with right-sided pleural thickening secondary to old tubercular effusion and managed conservatively with symptomatic treatment.
Conclusion- The colour Doppler application along with real-time chest ultrasound increases diagnostic accuracy to differentiate minimal effusion from pleural thickening hence should be an integral part of real-time ultrasound at the time of evaluation of minimal pleural fluid.
References
-
M. Kalokairinou, K. Maratou et al, Application of color Doppler ultrasound in the study of small pleural effusion, Med. Ultrasono. 12 (2010) 12–16.
-
Qureshi NR, Glesson FV. Imaging of pleural diseases. Clin Chest Med. 2006;27:193-213.
-
Feilfei Hou, Xingshun Qi, Zheng Ning et al. Prevalence, risk factor and in-hospital outcome of pleural effusion in liver cirrhosis: A retrospective observational study. Int J Clin Exp Med 2016;9(2):3265-327
-
Surekha B, Thukral BB, Mittal MK, Mittal A, Sinha M. Radiological review of pleural tumours. Indian JRadiol Imaging 2013;23:313-320.
-
T.H. Tsai, P.C. Yang, Ultrasound in the diagnosis and management of pleural disease, Curr. Opin. Pulm. Med. 9 (2003) 282–290.
-
P.C. Yang, K.T. Luh, et al , Value of sonography in determining the nature of pleural effusion: analysis of 320 cases, AJR Am. J. Roentgenol. 159 (1992) 29–33.
-
Hasan A, Makhlouf A, Mohamed R. Discrimination between pleural thickening and minimal pleural effusion using colour Doppler chest ultrasonography. Egyptian Journal of Chest Diseases and Tuberculosis. 2013 Jul 1;62(3):429-33.
-
Mitchell DG, Burns PN, Needleman L. Color Doppler artifact in anechoic regions. J Ultrasound Med 1990;9:255-60.