Hypoxemia After a Road Traffic Accident in Kenya
B Jason Brotherton, MD, MS1,2; Robert Kivindu, MBChB1; Kristina E. Rudd, MD, MPH3
1Department of Internal Medicine, Kijabe Hospital, Kijabe, Kenya
2Department of Critical Care, Kijabe Hospital, Kijabe, Kenya
3Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Case:
A previously healthy 22-year-old woman was transferred to our hospital in rural Kenya from an outside facility for a higher level of surgical care. One day prior to transfer she was involved in a road traffic accident, where she was a passenger on the back of a motorcycle. She sustained fractures of her right ischium, midshaft of the right femur, and distal right tibia and fibula. No other injuries were reported.
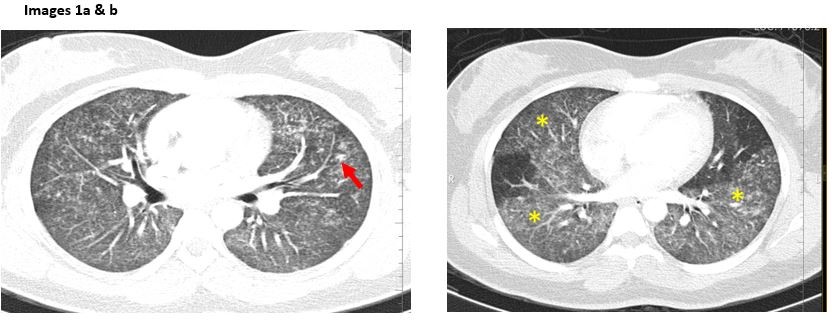
Shortly after arrival to our hospital she was noted to become newly tachypneic and hypoxemic. Vital signs at that time were the following: blood pressure 107/51 mm Hg, pulse 112 beats/min, respiratory rate 28 breaths/min, peripheral capillary oxygen saturation breathing ambient air 84%, and Glasgow Coma Scale 15. A computed tomography (CT) scan with intravenous contrast of the chest was obtained (Figures 1a, 1b) and a diagnosis was made.
Question:
Based on the history and CT findings, what is the most likely diagnosis?
- Pulmonary embolism
- Aspiration pneumonia
- Fat embolism
- Pulmonary contusion
C. Fat embolism
Discussion:
CT images of this patient revealed bilateral ground glass opacities (*) and patchy nodular infiltrates (red arrow). The pulmonary arteries showed no filling defect.
This patient was diagnosed with fat embolism, defined as the presence of fat globules in the pulmonary circulation. Fat embolism occurs in as many as 80% of patients with traumatic skeletal injuries, and long bone fractures are the most common associated injury.1 The underlying pathophysiology is not well understood, but there are two proposed mechanisms.2 The mechanical theory suggests that long bone injury forces fat globules out of the venous sinusoids into the circulation that then travel to the lungs and systemic circulation, causing occlusive injury. The biochemical theory posits that mobilized fat globules initiate a proinflammatory state. These inflammatory molecules are then hydrolyzed, releasing free fatty acids while simultaneously stimulating further cytokine release. This results in more peripheral tissue damage by generating vasogenic and cytotoxic edema.2
Symptoms from a fat embolism occur 12-72 hours after the initial insult. While fat embolism syndrome (FES) is classically described as a triad of respiratory distress, altered mental status, and petechial rash, none of these three signs are pathognomonic for the condition. Pulmonary manifestations of dyspnea, tachypnea, and hypoxia are the most common, occurring in 96% of cases of FES.1 Neurologic findings, including altered mental status, seizures, and focal neurologic deficits, are next most common, but are only present in 59% of patients with FES. Petechial rash occurs in non-dependent areas of the head, thorax and axilla. It is last to appear and least common, emerging in only 20% of cases.1
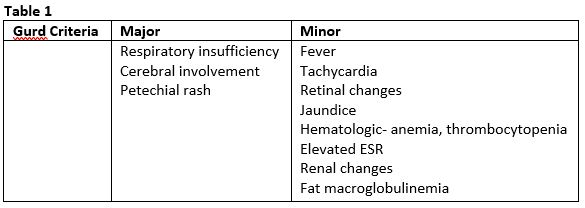
Historically diagnosis has been made clinically but there have been three different sets of criteria to devised to aid in diagnosing FES: Gurd’s, Schonfeld’s, and Lindeque’s criteria.1,2,3 These criteria were based upon separate, small clinical studies and have not been prospectively validated.1,2,3 Gurd’s criteria have been the most frequently used, and require 1 major and 4 minor criteria for diagnosis of FES (Table 1).2 There are no specific laboratory tests for FES, but frequently patients also present with anemia, thrombocytopenia, elevated ESR and CRP, or hypoalbuminemia.2 Our patient was diagnosed with fat embolism based upon her clinical presentation and radiographic imaging. She did not meet for the full criteria for FES.
Chest imaging can be beneficial in the correct clinical setting. Chest radiographs often have bilateral, diffuse patchy infiltrates resembling Acute Respiratory Distress Syndrome. CT scan of the chest, as in our patient, often shows bilateral ground glass opacities and consolidation with clear demarcation between areas of normal lung and areas of affected lung. Other CT findings can include “crazy paving” which is characterized by a reticular pattern superimposed on ground-glass opacities.4 The term is used because it resembles the appearance of paths made with broken pieces of stone. The extent of findings seen on CT scan have been correlated with severity of clinical disease.5 The bilateral, well demarcated ground glass opacities (*) , patchy nodular infiltrates (red arrow), and interlobular septal thickening (not depicted in our images) are characteristic of fat embolism.
Regarding the other options listed, the history, presentation, and CT findings made fat embolism most likely. The pre-test probability for pulmonary embolism was low given her lack of recent surgery, immobility for less than three days, likelihood of current symptoms being due to a diagnosis other than PE, and no prior history of deep vein thrombosis or PE. The pulmonary and segmental vessels were patent, which an occlusion to these vessels is the primary radiologic finding. Radiographic findings of aspiration pneumonias are often in gravity dependent areas.6 The diffuse location of the ground glass opacities and lack of history of loss of consciousness made aspiration pneumonia less likely. Pulmonary contusions are common in trauma patients, and often have similar symptom onset and appearance on radiography as patients with fat embolism. The key distinguishing factor on CT scan is that in pulmonary contusions, there is often 1-2 mm of sub-pleural sparing of the lung parenchyma adjacent to the thoracic wall injury not seen in fat embolism.7
There is no disease-specific, evidence-based management for fat embolism, but addressing the underlying etiology is imperative. Therapies such as heparin, intravenous fluids, corticosteroids, and aspirin have been tried previously, but none have proven to be of benefit. Despite the severity of initial presentation of these patients, the outcome is generally favorable, with mortality being less than 10% in the setting of early fixation of the fracture(s) and aggressive supportive care.1 Our patient had fixation of her multiple fractures, and experienced complete recovery from her respiratory distress over the following three days. She was discharged home in good condition one week later.
References
-
Kosova E, Bergmark B, Piazza G. Fat Embolism Syndrome. Circulation 2015; 131: 317-20.
-
Rothberg DL, Makarewich CA. Fat Embolism and Fat Embolism Syndrome. J Am Acad Orthop Surg 2019; 27: e346-e355.
-
Malagari K, Economopoulos N, Stoupis C, et. al. High-Resolution CT Findings in Mild Pulmonary Fat Embolism. CHEST 2003; 123: 1196–1201.
-
Lee CH. The Crazy Paving Sign. 2007; 243: 905-906.
-
Newbigin K, Souza CA, Armstrong M, et. al. Fat Embolism Syndrome: Do the CT findings correlate with clinical course and severity of symptoms? A clinical-radiological study. European Journal of Radiology 2016; 85(2): 422–7.
-
Lango DL. Aspiration Pneumonia. N Engl J Med 2019; 380: 651-63.
-
Požgain Z, et al. Pulmonary contusions after blunt chest trauma: clinical significance and evaluation of patient management. European Journal of Trauma and Emergency Surgery (2018) 44:773–777



