Nodules, Nodules – More to it than meets the eye
Srikant Kashinath Malegaonkar, MD
Post Graduate Institute of Medical Education and Research, Chandigarh
Case
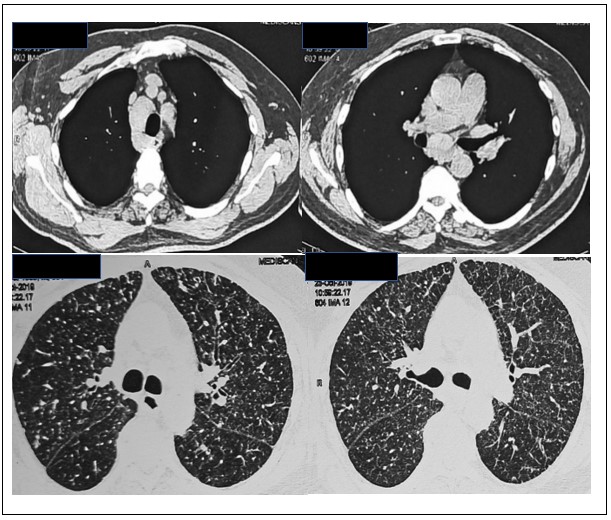
A 60-year-old gentleman with well controlled type 2 diabetes mellitus presented to the clinic with an episode of streaky haemoptysis. There were similar episodes of streaky haemoptysis in the past (about two episodes per year in the last three years) which would resolve with oral tranexamic acid within two to three days. There was no other significant history apart from one of his co-workers being treated for sputum positive tuberculosis. Vitals and physical exam were within normal limits. Laboratory results including complete blood count and coagulation profile were within normal limits. Induced sputum stain, culture and Xpert MTB/RIF were negative. Contrast enhanced computed tomography of chest along with high resolution parenchymal cuts of lung are depicted below.
Question
What would be the next best step in the management of the above patient?
- Start empirical anti tubercular treatment
- Bronchoscopy and sampling from abnormal areas
- Computed tomography pulmonary angiogram
- Continue oral tranexamic acid and observe
Which among the following are other presentation/s of the above disease?
- Septal thickening
- Pleural effusion
- Tracheobronchial plaque
- All of the above
Question 1 Answer
B. Bronchoscopy and sampling from abnormal areas
Question 2 Answer
D. All of the above
Discussion
Haemoptysis requires prompt evaluation to determine its underlying cause and initiation of appropriate therapy. Computed tomography patterns in combination with history and physical examination can help the clinician narrow the differential.(1) This patient imaging pattern demonstrated mediastinal lymphadenopathy at lower paratracheal (4R), subcarinal (7), bilateral hilar (10) stations along with diffuse perilymphatic nodules.
The differential for perilymphatic nodules include silicosis, sarcoidosis, amyloidosis and lymphangitic carcinomatosis.(2) Therefore, establishing a tissue diagnosis is critical for management. Miliary pulmonary tuberculosis presents with random micro-nodules on CT and would require microbiological evidence which was lacking in our patient (Question 1, answer A is incorrect). Due to concerns of diffuse parenchymal lung disease with ongoing haemoptysis observation with tranexamic acid would be inappropriate (Question 1, answer D is incorrect). CT pulmonary angiography (CTPA) is a good modality for patients with active haemoptysis but it would only convey to us the source of bleeding but not the underlying aetiology (Question, 1 answer C is incorrect).
Our patient underwent endobronchial ultrasound guided transbronchial needle aspiration from mediastinal lymph nodes along with endobronchial and transbronchial biopsies. Histopathology revealed amorphous material filling the interstitium with apple green birefringence with Congo red stain, consistent with amyloidosis.
Pulmonary amyloidosis is an uncommon disease that can present with a broad range of radiographic findings, such as diffuse alveolar septal involvement with perilymphatic lung nodules, interstitial involvement in form of septal thickening and mediastinal and hilar lymph node enlargement. Nodules and lymph nodes are often calcified. Diffuse alveolar septal amyloidosis is often associated with amyloid light chain (AL) amyloidosis. Other forms of pulmonary amyloidosis include tracheobronchial involvement with submucosal plaques, localised nodular amyloidosis and pleural effusion (Question 2 answer D). Ideally, tissue biopsies should be obtained from the least invasive sites (abdominal fat, minor salivary glands) due to an increased risk of bleeding in these patients. Once diagnosed, further treatment of pulmonary amyloidosis depends upon whether the disease is localised or systemic. Treatment options also depend upon the fibril protein type and underlying aetiology.(3)
Our patient underwent bone marrow aspiration and biopsy which revealed hypercellular marrow with clonal plasma cells constituting >1% of cell lines, abdominal fat pad biopsy stained positive for amyloid and serum free light chain assay was positive. A final diagnosis of AL amyloidosis secondary to plasma cell dyscrasia was made. Patient is currently on chemotherapy combination of bortezomib, lenalidomide and dexamethasone for this primary disease.
References
-
Ketai LH, Mohammed T-LH, Kirsch J, Kanne JP, Chung JH, Donnelly EF, et al. ACR appropriateness criteria® hemoptysis. Journal of thoracic imaging. 2014;29(3):W19-W22.
-
Criado E, Sánchez M, Ramírez J, Arguis P, de Caralt TM, Perea RJ, et al. Pulmonary sarcoidosis: typical and atypical manifestations at high-resolution CT with pathologic correlation. Radiographics. 2010;30(6):1567-86.
-
Milani P, Basset M, Russo F, Foli A, Palladini G, Merlini G. The lung in amyloidosis. European Respiratory Review. 2017;26(145).