"Sudden onset chest pain in a teenage boy"
Ashley Deschamp, M.D., M.S.
Pediatric Pulmonary Fellow
Nadia Krupp, MD
Assistant Professor of Clinical Pediatrics
Indiana University School of Medicine, Indianapolis, IN
Case:
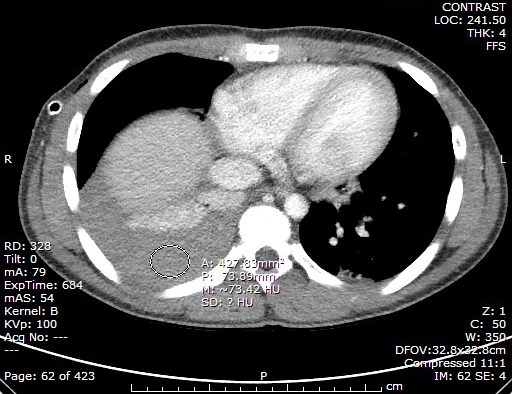
A previously healthy 13 year old male presented to the ER with a 1 day history of cough, right-sided chest pain, and dizziness. There was no recent illness, fever, travel, drug use, or sputum production. Physical examination demonstrated dullness to percussion and right-sided egophony on chest exam with no crackles or wheeze. Extremities were cool, capillary refill 3 seconds. CBC showed WBC 15.2 k/cumm (neutrophils 83%, lymphocytes 10%, monocytes 7%, eosinophils 1%, basophils 0%), hemoglobin 12.2 GM/dL, hematocrit (Hct) 36.8%, platelets 239 k/cumm. CT chest demonstrated the following:
Pleural fluid analysis revealed: grossly bloody, total nucleated cell count 3,850/cumm (54% neutrophils, 20% lymphocytes, 1% eosinophils, 25% monocytes), pleural fluid Hct 35%.
Question:
What is the diagnosis?
- Histoplasmosis
- Hemothorax
- Community acquired pneumonia with effusion
- Eosinophilic pneumonia
Correct answer: B
Discussion:
Hemothorax can be divided into two categories, traumatic and spontaneous. The majority of cases of hemothorax are related to trauma, the incidence of which is estimated to be 1 in 300,000 cases per year. Spontaneous hemothorax is much less common, mainly described in case reports and case series. Some of the potential etiologies of spontaneous hemothorax include congenital and acquired coagulopathies, vascular malformations, neoplasms, and rare causes such as endometriosis and pulmonary sequestration.5
Rarely, a cause is not identified and the case remains idiopathic. Investigation of underlying causes may include chest x-ray, contrast enhanced chest CT or CT angiogram, echocardiogram with bubble study, coagulation parameters, pleural cytology, thorascopic exploration and pleural biopsy.
In most cases, placement and drainage of the hemothorax with a large diameter (>= 24Fr) chest tube is an adequate initial treatment approach. In those with hemodynamic instability, thoracotomy is the procedure of choice. Video assisted thorascopy (VATS) may be considered in those with active blood loss but stable hemodynamics as well as when there is > 500 mL of blood or blood filling >= 1/3 of the hemi-thorax. Other interventions include correction of coagulopathy if present. If the hemothorax is loculated, intrapleural fibrinolytic therapy (IPFT) is an option with tPA, urokinase, or streptokinase. In most trials, this is initiated at least 4 days after the onset of hemothorax if blood remains despite chest tube drainage. Adequate drainage is required as retention of blood in the pleural cavity can lead to lung entrapment, chronic fibrothorax, impaired lung function and infection.
References:
- Broderick SR. Hemothorax Etiology, Diagnosis, and Management. Thorac Surg Clin 2013; 23: 89-96.
- Yalcin NG et al. Anatomy and Pathophysiology of the Pleural and Pleural Space. Thorac Surg Clin 2013; 23: 1-10.
- Boersma WG et al. Treatment of Hemothorax. Respir Med 2010; 104: 1583-87.
- Calvin SH et al. Spontaneous Hemothorax: What is in a name? World J Surg 2009; 33: 1780-81.
- Hakim AA et al. Spontaneous Hemothorax A Comprehensive Review. CHEST 2008; 134: 1056-65.



