The White Plague
Mohamad Badr Jandali, MD & Deepika Polineni, MD
Kansas University Medical Center, Department of Pulmonary and critical care Medicine
Case
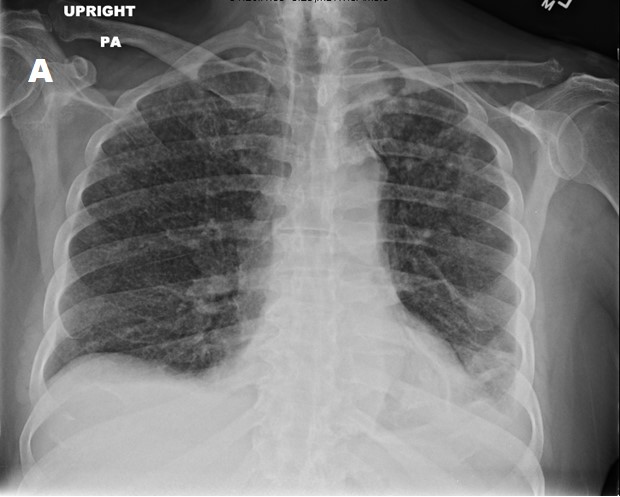
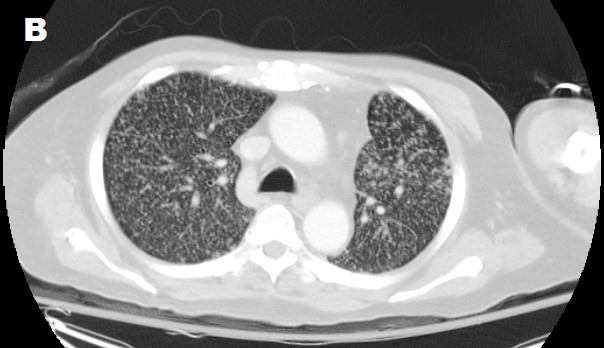
A 52-year-old male from Mexico with advanced alcoholic liver disease presented with confusion, cough, and mild hemoptysis. The patient endorsed daily alcohol consumption and a prior smoking history, but denied recreational drug abuse. Vitals showed a temperature of 38.1 C and labs showed acute on chronic hyponatremia to 119 mmol/L and severe thrombocytopenia to 4 K/UL. His chest X-ray (image A) and CT scan (image B) are shown below.
Images
Question
What is the most likely diagnosis?
- Miliary Tuberculosis
- Septic emboli
- Malignant metastases
- Sarcoidosis
Answer: A. Miliary Tuberculosis
Discussion
These are classic radiographic findings of miliary tuberculosis (TB). A miliary pattern is characterized by innumerable small diffuse nodular densities throughout lung fields, usually 1-3mm in diameter[1]. In the nineteenth century, TB was called the white plague as patients became extremely pale before death. History and clinical suspicion should guide the work up of miliary radiographic pattern. In our patient, a diagnosis of TB was established with a positive T-spot followed by positive peritoneal fluid AFB cultures.
The term miliary opacities comes from the appearance of the millet seed, a common grain grown around the world (image C). While the radiographic miliary pattern is most commonly linked to tuberculosis, but it can actually be seen in many other diseases: infections such as tuberculosis, Haemophilus influenza, Mycoplasma pneumonia, and fungal infections [2]; metastatic malignancy such as papillary thyroid cancer, renal cell carcinoma, lymphoma, and osteosarcoma [3]; and other conditions including sarcoidosis, hypersensitivity pneumonitis, and pneumoconiosis.
The treatment of miliary or disseminated tuberculosis is similar to that of pulmonary TB. It starts with 4 drug intensive phase therapy with Isoniazid, Rifampin, Pyrazinamide and Ethambutol for 8 weeks followed by 18 weeks of 2 drug continuation therapy with Isoniazid and Rifampin. The role of adjunct corticosteroid therapy remains controversial, but it should be considered especially when CNS involvement is present. Seeking an expert opinion is strongly recommended, as many of these patients require individualized therapy regimens due to certain comorbidities. Prognosis largely depends on baseline comorbidities, treatment adherence and organ involvement where CNS disease seems to predict higher mortality [4]. Unfortunately, our patient's condition worsened despite therapy and he died from multiorgan failure.

References:
-
Andreu J, et al. Miliary lung disease revisited. Curr Probl Diagn Radiol 2002; 31(5): 189-97.
-
Furqan M and Butler J. Miliary pattern on chest radiography: TB or not TB? Mayo Clin Proc 2010. 85(2): 108.
-
Koutsopoulos AV, et al. Is a miliary chest pattern always indicative of tuberculosis or malignancy? Respiration, 2006; 73(3): 379-81.
-
Nahid P, et al. Official American Thoracic Society / Centers for Disease Control and Prevention / Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of drug-susceptible tuberculosis. Clin Infect Dis 2016; 63(7): e147-95.



