To Cath or Not to Cath?
Georgios A. Triantafyllou MD1, Andrew W. Swartz MD2, Mohamed A. Hassan MD2, Burton W. Lee1
From the Division of Pulmonary, Allergy, and Critical Care Medicine (1), and the Department of Medicine (2), both at the University of Pittsburgh Medical Center
Case:
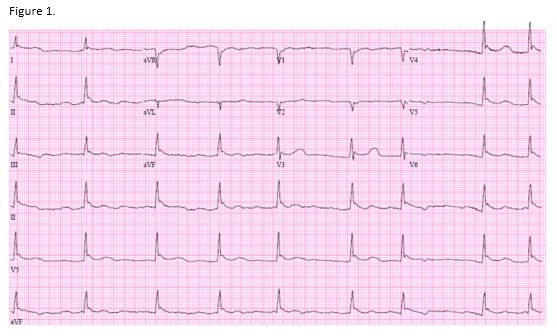
A 52-year-old woman was brought to the emergency room after she was found unresponsive outside of her house. Her temperature was 25.2oC and an arterial blood gas showed severe metabolic and respiratory acidosis (pH 7.0), with a lactate of 7.2. An EKG is shown below. An initial troponin is negative.
Question:
What is the next best step?
- Activate the cath lab for left heart catheterization
- Administer tPA
- Initiate active core rewarming, be prepared for ACLS as this patient is at high risk for ventricular fibrillation
- Initiate active core rewarming, this EKG shows a benign finding which will resolve after she reaches normothermia
C. Initiate active core rewarming, be prepared for ACLS as this patient is at high risk for ventricular fibrillation
Discussion:
EKG reveals Osborn waves (Figure 1.). With active rewarming, the Osborn waves became less pronounced and eventually resolved. Interestingly, normalization of her pH did not affect the EKG changes, as those lingered when her temperature was 30.2 oC and her pH was 7.43.
Osborn (or J) waves were named after John Osborn who described their presence as a herald of ventricular fibrillation in hypothermic dogs. They are defined as a positive deflection at the J point (1). Hypothermia increases the ratio of the conduction time to the refractory period, rendering the heart more prone to ventricular fibrillation. Sympathomimetic amines can decrease the conduction time by increasing the conduction velocity. They may be used to decrease the incidence of ventricular fibrillation, although data regarding their use in humans are lacking (2). Finally, Osborn waves can also be seen in early repolarization, increased vagal tone, hypercalcemia, and Brugada syndrome. Their presence can be benign or associated with increased risk for ventricular fibrillation (3). Clinicians should always interpret their presence in the right clinical context, especially since they are frequently interpreted as “ST elevation/acute myocardial infarction” by the ECG machine.

Figure 2. Osborn (J) waves can be seen in leads V4-V6 (arrows). The prominence of these waves gradually decreased with rising temperature and resolved when patient reached normothermia. However, normalization of the pH did not lead to resolution of the J waves (middle panel).
References:
-
Osborn JJ. Experimental hypothermia; respiratory and blood pH changes in relation to cardiac function. The American journal of physiology 1953; 175: 389-398.
-
Covino BG, D'Amato HE. Mechanism of ventricular fibrillation in hypothermia. Circulation research 1962; 10: 148-155.
-
Junttila MJ, Sager SJ, Tikkanen JT, Anttonen O, Huikuri HV, Myerburg RJ. Clinical significance of variants of J-points and J-waves: early repolarization patterns and risk. European heart journal 2012; 33: 2639-2643.



