Contributed by Deepa Burman MD1,2; Thomas Rice MD1; Charles Atwood MD1,2 Institutions: 1. VA Pittsburgh Healthcare System 2. University of Pittsburgh Medical Center Corresponding Author: Deepa Burman MD Phone number: 412 673 5504 Email id: burmand@upmc.edu Contributions: All authors reviewed the case and worked on editing the manuscript. Dr Burman prepared the manuscript in addition to case review. Source of support: None Mesh Terms: Artifacts, sleep disorders
In Brief
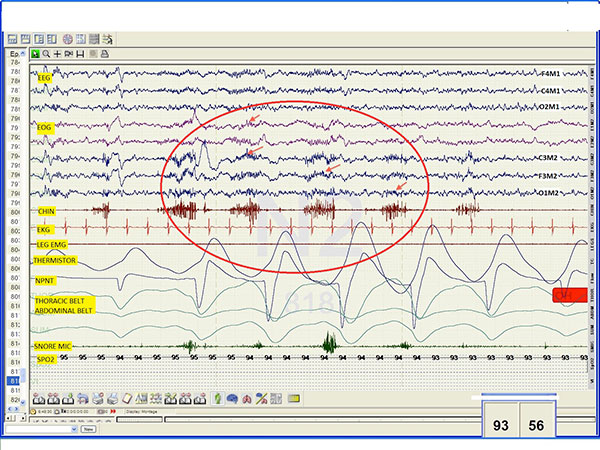
60 year old male with excessive daytime sleepiness with EEG and EMG abnormalities on a polysomnogram.
Case Vignette
A 60 year old man with a medical history of hypertension presented to the sleep lab with excessive daytime sleepiness, mild snoring and witnessed apneas. The technician noted presence of left sided facial twitching during the set up. The diagnostic PSG revealed moderate OSA. In addition, the patient was noted to have an unusual finding throughout the sleep study. See Image
Polysomnogram Tracing:
Questions
What is the most likely cause of the abnormality noted on the polysomnogram segment?
- Sleep Spindles
- Bruxism
- Snore artifact
- Artifact from left sided hemi-facial muscle spasm
- Seizure activity
Answer:
Artifact from left sided hemi-facial muscle spasm
Discussion:
The patient was found to have an artifact in the left sided EEG signals from unilateral facial muscle twitching throughout the study. It was worse in wake stage and disappeared in REM (likely related to muscle hypotonia in REM sleep). The video recording was not clear enough to identify the twitching. But, the set up technician noted facial twitching on left side while hooking up the patient with electrodes and commented on it so that we can keep that in mind while reviewing the study that the facial twitch could possibly cause some artifact in the study.
The patient had increased chin activity and increased EEG frequencies at irregular intervals. Some, but not all, of those abnormalities corresponded to snoring on the snore channel. The increased EEG frequency was mostly noted on left side frontal and central EEG channels and less so in the occipital and right sided channels.
The artifact shown is not a spindle activity because it does not meet the frequency criteria (11-16 Hz; maximal in central leads) and the maximum amplitude is noted in the EMG channel 1.
It is unlikely to be a snore artifact because only a few but not all events lined up with snoring and there was no evidence of snore artifact in the nasal pressure channel 2. The filters used on nasal transducer and snore mic were as follows: NPNT: HFF 5 Hz and LFF 0.1 Hz. Snore mic: HFF 70 Hz, and LFF 10 Hz. Since we used non-standard filters on the on the nasal pressure transducer (AASM recommendation: No filter if a DC channel or <0.01 and 100Hz) snoring artifact is still a slim possibility. However snoring was also recorded using a microphone and was specifically commented on by the technician to be absent.
Although the events meet some PSG criteria for bruxism like elevation of chin EMG for 0.25 to 2 seconds at least twice the amplitude of background EMG; it is unlikely to be bruxism because of the laterality and absence audio evidence of tooth grinding as heard during the recording or commented upon by the technicians 3,4.
The epoch was changed to a 10-second window to look for seizure activity. The artifact is unlikely to be a seizure because it does not meet the spike (transient with pointed peak and duration of 20-70 msec) or polyspike (multiple spikes) criteria for ictal activity. Unfortunately, we did not obtain a picture of the 10-second window of the artifact to prove that.
Our patient had hemi-facial spasm (HFS) characterized by chronic twitching of one side of the face. It affects muscles innervated by the motor branch of the facial nerve. HFS is believed to result from irritation of the facial nerve at its exit from the brainstem and most cases are associated with compression by a small vascular loop. It is sometimes associated with vertebral artery dolichoectasia 5.
Vascular dolichoectasia refers to elongation and distention of blood vessels. The most common cause is hypertension. When the affected blood vessel is the vertebrobasilar artery, it can result in hemifacial spasm, trigeminal neuralgia or facial paresis.
Careful review of PSG and medical history is essential to recognize the exact cause of an artifact which allows for correct interpretation of polysomnogram.
Follow up: The patient had been evaluated by a neurologist for his facial twitching and was considering Botox injections for symptom relief. Patient had not undergone Botox treatment and so comparison PSG pre and post botox is unavailable to date.
References:
1 Iber C, author; American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 2007. Westchester, IL: American Academy of Sleep Medicine;
2 Harris CD, Dexter D: Recording artifacts.
3,4 American Academy of Sleep Medicine. The international classification of sleep disorders. 2nd ed. Westchester: American Academy of Sleep Medicine, 2005.
Carra MC, Huynh N, Lavigne, G: Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Dent Clin North Am. 2012 Apr;56(2):387-413.
5 Arantes M, Garcia R, Pereira JR, Costa M: Hemifacial spasms and vertebral dolichoectasias. Revista De Neurologica 2008 Nov 1-15;47(9):468-70.